Does Depression Accelerate Aging? The Link Between Mental Health and Disease Risk
Mental health isn’t just “in your head.” Increasingly, science shows that conditions like depression are deeply connected to our biology, affecting everything from cellular aging to the risk of chronic illnesses such as heart disease and diabetes. Recognizing this mind-body link helps us move past stigma and adopt comprehensive strategies for mental and physical health.
In this article, we’ll examine the fascinating science behind depression and accelerated aging, explore how mental health disorders increase the risk of physical illness, and emphasize why addressing both mind and body is crucial for long-term health.
Depression and Biological Aging: What the Science Shows
Depression is one of the most common mental health disorders worldwide, affecting over 300 million people. But beyond the emotional and cognitive symptoms, depression impacts the body at a cellular level. Researchers now see depression not only as a mental health disorder but also as a condition of accelerated biological aging.
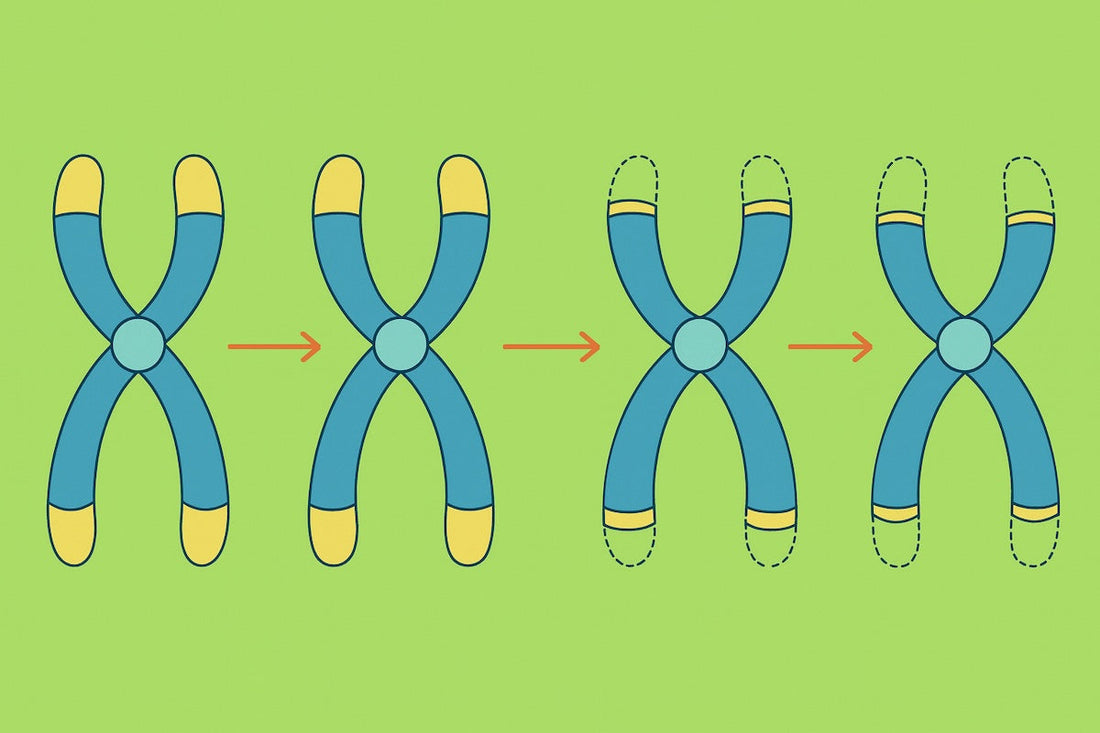
Telomere Shortening
Telomeres are protective caps at the ends of chromosomes that naturally shorten with age. Shorter telomeres are linked to age-related diseases and a higher risk of early death. Multiple studies have shown that people with major depressive disorder (MDD) often have shorter telomeres than their non-depressed counterparts.
- In one landmark study, researchers found that the total length of depression duration was directly linked to telomere shortening.
- A 2025 meta-analysis of 71 studies confirmed a significant connection between depression and reduced telomere length.
Epigenetic Clocks
Another method scientists use to measure biological age is through DNA methylation patterns (epigenetic clocks). These clocks often show that individuals with depression have a “biological age” older than their chronological age, a phenomenon called epigenetic age acceleration.
For example, a study in Nature Communications (2023) showed that not only can depression accelerate biological aging, but also that accelerated aging might predispose individuals to develop depression — a bidirectional relationship.
Inflammation and Oxidative Stress
Depression is closely linked to chronic inflammation. Elevated levels of inflammatory cytokines and oxidative stress markers damage cells and DNA, which speeds up aging processes. This biological stress may partly explain why depression is associated with higher rates of age-related diseases such as dementia, cardiovascular disease, and cancer.
Depression and Physical Health: A Two-Way Street
The consequences of depression don’t stop at aging markers. People with depression are more likely to develop serious medical conditions. In turn, chronic diseases can worsen mental health, creating a vicious cycle.
Depression and Heart Disease
People with depression have a 64% higher risk of developing coronary artery disease.
Depression after a heart attack is common and predicts worse outcomes, including higher rates of rehospitalization and mortality.
Biological mechanisms include increased inflammation, dysregulated stress hormones, and unhealthy lifestyle factors like poor sleep, smoking, or inactivity.
Depression and Diabetes
Research shows that depression increases the risk of developing type 2 diabetes by up to 60%.
Depression may contribute to insulin resistance through elevated cortisol levels, inflammation, and disrupted circadian rhythms.
Conversely, living with diabetes — with its daily demands and complications — can also trigger or worsen depression, highlighting the bi-directional link.
Depression and Chronic Pain
Chronic pain conditions (like fibromyalgia, arthritis, or neuropathy) often co-occur with depression.
The shared pathways include inflammation, altered pain perception, and neurotransmitter imbalances.
Depression can lower pain tolerance, while constant pain can worsen mood — another feedback loop that erodes quality of life.
Depression and Neurodegenerative Disease
Late-life depression is a known risk factor for dementia, including Alzheimer’s disease.
Accelerated aging in the brain, vascular damage, and neuroinflammation may connect the dots between mood disorders and cognitive decline.
Other Mental Health Conditions and Accelerated Aging
Depression isn’t the only condition tied to accelerated aging. Research suggests a similar pattern in related disorders:
- Post-Traumatic Stress Disorder (PTSD): Linked with shorter telomeres, higher inflammation, and accelerated brain aging.
- Anxiety Disorders: Associated with elevated stress hormones and systemic inflammation, which can both contribute to earlier biological aging.
- Bipolar Disorder: Patients often show age-related conditions earlier in life, including metabolic syndrome, cardiovascular disease, and cognitive decline.
These findings suggest that mental health conditions broadly impact the biology of aging, not just mood.
Why Does Mental Illness Accelerate Aging?
Scientists are piecing together several overlapping mechanisms:
- Chronic Stress and Cortisol: Long-term activation of the body’s stress response damages cells, promotes inflammation, and disrupts metabolism.
- Inflammation and Immune Dysfunction: “Inflammaging” — the persistent low-grade inflammation linked to both aging and mental illness — speeds up tissue damage.
- Oxidative Stress: Excess free radicals harm DNA, proteins, and lipids, accelerating cellular wear and tear.
- Mitochondrial Dysfunction: The cell's powerhouses deteriorate more quickly under chronic stress and depression, impairing energy production.
- Lifestyle Factors: Depression often decreases motivation for exercise, healthy eating, and sleep hygiene — behaviors vital for slowing aging.
A Holistic Approach to Slowing the Clock
Here's the good news: accelerated aging associated with depression is not permanent. Research indicates that with proper treatment and lifestyle adjustments, biological aging indicators like telomere length and epigenetic age can either stabilize or improve.
Mental Health Treatment
Psychotherapy (e.g., CBT, ketamine-assisted psychotherapy, EMDR for trauma) can help address underlying issues.
Medication and innovative treatments (antidepressants, ketamine therapy, Spravato) reduce symptoms and may help normalize biological stress responses.
Lifestyle Interventions
Exercise: Regular physical activity is one of the strongest protectors against both depression and aging.
Nutrition: Diets rich in whole foods, antioxidants, and omega-3 fatty acids fight oxidative stress and inflammation.
Sleep hygiene: Consistent, restorative sleep supports both mental health and cellular repair.
Mind-body practices: Meditation, mindfulness, and breathwork calm the stress response and lower inflammation.
Social Connection
Loneliness itself is a risk factor for both depression and faster aging. Maintaining strong social bonds offers emotional resilience and biological protection.
The Takeaway: Mind and Body Are One
Depression and other mental health conditions don’t just influence mood — they also affect the body, accelerating aging and raising the risk of chronic illnesses. Recognizing this link opens the door to more holistic, compassionate care.
Treating depression isn’t only about improving mental health; it’s about increasing healthspan — the years we live in good health. By addressing both mind and body through therapy, lifestyle changes, and medical care, we can help slow aging and build resilience for the future.
Disclaimer:
The content provided on this blog and website is for educational and informational purposes only and should not be considered medical advice. Newy supplements are not intended to diagnose, treat, cure, or prevent any disease. Always consult a qualified healthcare professional before starting any new supplement, especially if you are pregnant, nursing, have a medical condition, or are taking other medications.
Resources:
Bair, Matthew J., et al. “Depression and Pain Comorbidity: A Literature Review.” Archives of Internal Medicine, vol. 163, no. 20, 2003, pp. 2433–2445. doi:10.1001/archinte.163.20.2433.
Gao, Y., et al. “Accelerated Biological Aging and Risk of Depression.” Nature Communications, vol. 14, 2023, Article 38013. doi:10.1038/s41467-023-38013-7.
Harvanek, Zachary M et al. “The Cutting Edge of Epigenetic Clocks: In Search of Mechanisms Linking Aging and Mental Health.” Biological psychiatry vol. 94,9 (2023): 694-705. doi:10.1016/j.biopsych.2023.02.001
Ismail, K., et al. “Exploring the Association between Depression and Telomere Length: A Meta-Analysis.” Scientific Reports, vol. 15, 2025, Article 7076. doi:10.1038/s41598-025-07076-5.
Karabatsiakis, Andreas, et al. “Telomere Shortening in Leukocyte Subpopulations in Depression.” BMC Psychiatry, vol. 14, 2014, Article 192. doi:10.1186/1471-244X-14-192.
Lavretsky, Helen. “Does Late-Life Depression Accelerate Aging?.” The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry vol. 31,1 (2023): 10-13. doi:10.1016/j.jagp.2022.09.003
Mezuk, Briana, et al. “Depression and Type 2 Diabetes over the Lifespan: A Meta-Analysis.” Diabetes Care, vol. 31, no. 12, 2008, pp. 2383–2390. doi:10.2337/dc08-0985.
Mendes-Silva, Ana Paula, et al. “Telomere Shortening in Late-Life Depression: A Potential Link with Disease Severity.” Brain and Behavior, vol. 11, no. 5, 2021, e2255. doi:10.1002/brb3.2255.
Ownby, Raymond L., et al. “Depression and Risk for Alzheimer Disease: Systematic Review, Meta-Analysis, and Metaregression Analysis.” Archives of General Psychiatry, vol. 63, no. 5, 2006, pp. 530–538. doi:10.1001/archpsyc.63.5.530.
Penninx, Brenda W J H. “Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms.” Neuroscience and biobehavioral reviews vol. 74,Pt B (2017): 277-286. doi:10.1016/j.neubiorev.2016.07.003
Rampersaud, R., et al. “Shorter Telomere Length Predicts Poor Antidepressant Response.” Scientific Reports, vol. 13, 2023, Article 8069. doi:10.1038/s41598-023-35912-z.
Verhoeven, Josine E., et al. “Major Depressive Disorder and Accelerated Cellular Aging: Results from a Large Psychiatric Cohort Study.” Molecular Psychiatry, vol. 19, no. 8, 2014, pp. 895–901. doi:10.1038/mp.2013.151.
Vakonaki, E et al. “Common mental disorders and association with telomere length.” Biomedical reports vol. 8,2 (2018): 111-116. doi:10.3892/br.2018.1040
Wolkowitz, Owen M., et al. “Leukocyte Telomere Length in Major Depression: Correlations with Chronicity, Inflammation and Oxidative Stress—Preliminary Findings.” PLoS ONE, vol. 6, no. 3, 2011, e17837. doi:10.1371/journal.pone.0017837.




