Neuroinflammation: Causes, Symptoms, and Natural Treatments
Inflammation is an essential defense mechanism that keeps us alive and healthy. However, issues occur when inflammation is unchecked, improperly triggered—as in autoimmune diseases—or spreads throughout the body, impacting vital organs. When this happens in the brain and central nervous system, it’s called neuroinflammation.
Neuroinflammation is increasingly recognized for its involvement in cognitive decline, mood disorders like depression and anxiety, and even neurodegenerative diseases. Typical signs can include brain fog, mental sluggishness, or heightened sensitivity to stress. While these symptoms seem mild, they may indicate a more serious issue.
The good news is that neuroinflammation can often be managed. By understanding its causes and triggers, we can take meaningful steps to reduce it naturally. In this article, we’ll explore what neuroinflammation is, what causes it, the symptoms to watch for, and practical, science-backed ways you can support your brain’s natural healing process.
What is Neuroinflammation?
Neuroinflammation is the inflammation in the central nervous system (CNS), which includes the brain and spinal cord. This response is usually triggered by the body’s immune system in reaction to infection, injury, toxins, or stress.
In small amounts, inflammation can be protective — it helps the brain heal from injury or infection. But when it becomes chronic, it can cause long-term damage and dysfunction. That’s when symptoms appear, and diseases can start to develop.
The brain's immune cells, especially microglia and astrocytes, have a significant role. When they are persistently activated, these cells release inflammatory cytokines, free radicals, and other molecules that can damage neurons and disrupt communication between brain cells.
What Causes Neuroinflammation?
1. Chronic Stress
Stress leads to a continuous release of cortisol and other stress hormones, which can interfere with brain signaling and weaken the blood-brain barrier, permitting inflammatory molecules to enter the brain.
2. Poor Diet
A diet high in refined sugars, processed foods, and industrial seed oils promotes systemic inflammation and harms gut health, both of which affect the brain.
3. Infections
Persistent infections, such as viral infections, Lyme disease, or even autoimmune reactions like PANDAS (a condition triggered by streptococcal infections), can provoke a continuous immune response in the brain—especially if the immune system is weakened.
4. Toxins and Environmental Pollutants
Exposure to heavy metals, mold, pesticides, and other toxins can trigger an inflammatory response in neural tissues. For instance, mercury and lead have been associated with cognitive decline and neuroinflammation; mycotoxins from black mold can compromise the blood-brain barrier and activate chronic immune responses; organophosphate pesticides are known to harm neuronal signaling; and airborne pollutants like fine particulate matter can enter the brain and promote inflammatory cascades.
5. Gut-Brain Axis Dysfunction
Your gut and brain are closely connected. When the gut becomes inflamed (a condition often called leaky gut), tiny gaps form in the intestinal lining. This allows bacteria, endotoxins like lipopolysaccharides (LPS), and undigested food particles to “translocate” into the bloodstream—where they shouldn’t be. Once in circulation, these substances can trigger a whole-body immune response and weaken the blood-brain barrier. The result is a chain reaction of inflammation that doesn’t stay only in the gut—it spreads to the brain, contributing to symptoms like brain fog, fatigue, anxiety, and depression.
6. Autoimmune Conditions
In some cases, the immune system mistakenly attacks the nervous system, leading to conditions like multiple sclerosis (MS) or autoimmune encephalitis.
Symptoms of Neuroinflammation
Neuroinflammation doesn’t always present with obvious, dramatic warning signs. Instead, it often develops subtly, gradually affecting daily life in ways that can easily be mistaken for stress, aging, or lifestyle factors. Because of this, many people live with ongoing brain inflammation without realizing it, dismissing their symptoms as “normal.”
Common signs to watch for include:
- Brain fog
- Memory issues or forgetfulness
- Chronic fatigue
- Anxiety and/or depression
- Headaches or migraines
- Sleep disturbances
- Light or sound sensitivity
- Trouble concentrating
While occasional experiences of these symptoms are normal, persistent or combined symptoms may indicate that the brain’s immune system is overactive. If left untreated, chronic neuroinflammation can disrupt mental clarity, mood regulation, and overall cognitive health, and over time, it has been associated with more serious conditions such as neurodegenerative diseases.
How Neuroinflammation is Linked to Chronic Disease
Scientists are increasingly discovering that chronic neuroinflammation is not just a symptom of brain dysfunction but a key factor behind many serious neurological and psychiatric conditions. For example, in Alzheimer’s disease and cognitive decline, activated immune cells in the brain (microglia) release inflammatory chemicals that damage neurons and speed up memory loss.
In Parkinson’s disease, similar inflammatory pathways contribute to the breakdown of dopamine-producing cells, worsening movement problems and mood shifts. Multiple sclerosis (MS) is also closely linked to neuroinflammation, where the immune system mistakenly attacks the protective myelin sheath around nerve fibers, disrupting communication between the brain and body.
Beyond these neurodegenerative diseases, research suggests that neuroinflammation also plays a role in autism spectrum disorder (ASD), affecting brain development and sensory processing, as well as in long COVID, where lingering inflammation may cause brain fog, fatigue, and other neurological symptoms. Mental health conditions are not exempt—depression, anxiety, and post-traumatic stress disorder (PTSD) are increasingly linked to inflammation in brain circuits that control mood and stress responses.
How to Test for Neuroinflammation
Currently, there is no single, simple at-home test that can definitively diagnose neuroinflammation. However, clinicians and functional medicine practitioners use a combination of tools to gather evidence that the brain’s immune system is activated:
- Blood markers: C-reactive protein (CRP), cytokines like IL-6, TNF-alpha
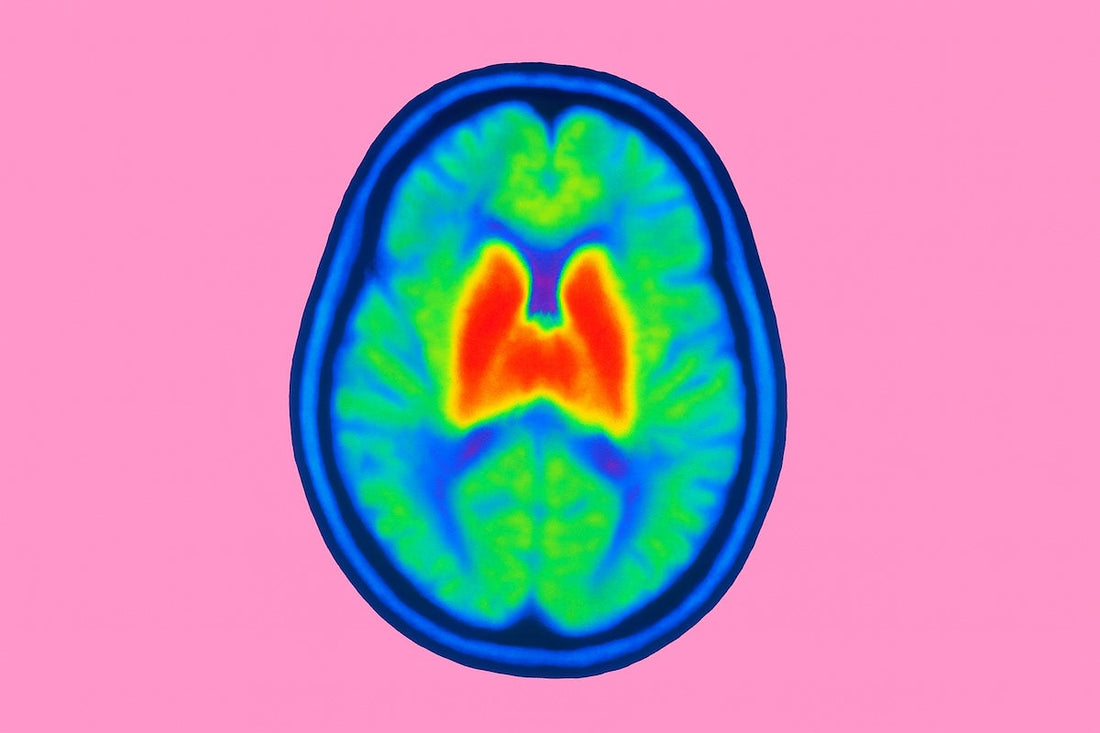
- Advanced imaging: PET scans that detect microglial activation
- Cognitive assessments and symptom tracking
Since many of these methods are not practical for daily use, individuals concerned about brain inflammation can still gain benefits by tracking their symptoms and focusing on anti-inflammatory strategies through nutrition, lifestyle, and targeted supplements. This allows patients to actively support brain health while collaborating with a healthcare provider for more comprehensive testing if needed.
How to Reduce Neuroinflammation Naturally
Fortunately, proven lifestyle changes and nutrients can reduce inflammation and restore brain balance. Here’s how you can begin healing your brain from the inside out:
1. Eat an Anti-Inflammatory Diet
Focus on whole, nutrient-dense foods that support the brain:
- Fatty fish (salmon, sardines) – rich in omega-3s
- Berries – high in polyphenols and antioxidants
- Leafy greens – loaded with vitamins and minerals
- Turmeric – contains curcumin, a powerful anti-inflammatory compound
- Fermented foods – support a healthy gut microbiome
Avoid:
- Refined sugar
- Processed carbs
- Vegetable oils (canola, soybean)
- Artificial additives and preservatives
2. Move Regularly
Moderate, consistent exercise helps reduce inflammation and promotes neurogenesis (the growth of new brain cells). Aim for 30 minutes of activity most days—such as walking, yoga, cycling, or resistance training.
3. Prioritize Sleep
Sleep is when your brain removes toxins through the glymphatic system. Poor sleep raises inflammation and hinders healing. Aim for 7–9 hours each night and cut down on screen time before bed.
4. Manage Stress Effectively
Chronic stress is a major driver of neuroinflammation. Try:
- Meditation or mindfulness
- Breathwork
- Nature walks
- Journaling
- Limiting toxic news and social media
5. Reduce Toxin Exposure
- Use a HEPA air purifier at home
- Drink filtered water
- Eat organic where possible
- Minimize plastic use
- Address mold issues if you suspect exposure
Supplements That Support Brain Inflammation
Some nutrients and natural compounds have been researched for their potential to reduce brain inflammation, safeguard neurons, and support recovery. Although supplements can't replace medical care, they can be a valuable addition to lifestyle adjustments and professional treatment.
Omega-3s (DHA & EPA) – Found in fish oil and algae, these essential fatty acids lower inflammatory cytokines, support the structure of brain cell membranes, and are closely associated with improved mood and cognitive function.
Curcumin – The active compound in turmeric, curcumin, can cross the blood–brain barrier, where it reduces oxidative stress and helps regulate microglial activity, potentially lowering the risk of neurodegenerative changes.
Magnesium L-threonate – A unique form of magnesium proven to penetrate the brain more effectively than other types, supporting synaptic plasticity, memory, and neuron repair stressed by inflammation.
Resveratrol – A polyphenol found in grapes and berries, resveratrol serves as both an antioxidant and anti-inflammatory, helping to protect the brain from oxidative damage related to aging and stress.
Alpha-Lipoic Acid (ALA) – A powerful antioxidant that functions in both fat- and water-soluble environments, ALA helps regenerate other antioxidants like glutathione and vitamin C, enhances mitochondrial function, and reduces oxidative stress linked to neuroinflammation.
Probiotics – By restoring balance in the gut microbiome, probiotics can reduce systemic inflammation, strengthen the gut-brain axis, and decrease the translocation of toxins that contribute to brain inflammation.
Note: Always consult a qualified healthcare provider before starting new supplements—especially if you’re on medications—as interactions and dosing considerations are unique to each person.
Heal Your Brain, Transform Your Life
Neuroinflammation isn’t always obvious, but its effects are real—showing up in your focus, mood, energy, and overall mental clarity. The good news? You don’t need a complicated protocol or a medical degree to start making a difference.
By nourishing your brain with anti-inflammatory foods, staying active, managing stress, and supporting your system with targeted nutrients, you give yourself the opportunity to think more clearly, feel more balanced, and fully engage in your life.
Your brain is adaptable. It wants to heal. And with the right care, it definitely can.
Disclaimer:
The content provided on this blog and website is for educational and informational purposes only and should not be considered medical advice. Newy supplements are not intended to diagnose, treat, cure, or prevent any disease. Always consult a qualified healthcare professional before starting any new supplement, especially if you are pregnant, nursing, have a medical condition, or are taking other medications.




